Prostate cancer represents a prevalent malignancy among men globally, originating in the prostate gland, a diminutive, walnut-shaped gland integral to the male reproductive system and responsible for the production of seminal fluid. While prostate cancer is often characterized by indolent progression and localized confinement, instances of aggressive behavior and metastasis to distal sites within the body are observed. This article aims to provide a thorough exposition of prostate cancer, encompassing its etiology, risk determinants, clinical manifestations, diagnostic modalities, therapeutic strategies, and preventive measures.
Prostate Gland Physiology and Prostate Cancer Pathogenesis
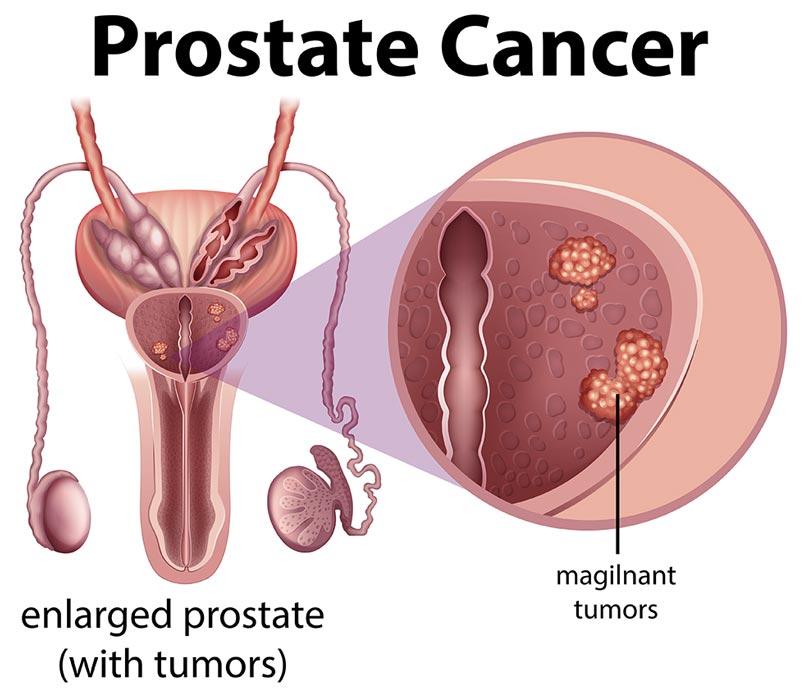
The prostate gland is anatomically situated inferior to the urinary bladder and encircles the urethra, the conduit for both urine and semen excretion. Prostate cancer arises from the aberrant proliferation of prostatic cells, leading to the formation of neoplastic masses. These malignant cells may extend beyond the confines of the prostate gland, invading adjacent tissues, regional lymph nodes, or distant organs, most commonly bone.
Prostate cancer is broadly classified into two principal categories based on the extent of disease dissemination:
- Localized Prostate Cancer: Malignancy confined exclusively within the prostate gland.
- Advanced Prostate Cancer: Malignancy that has extended beyond the prostate gland to distant anatomical sites.
Etiology and Predisposing Factors
The precise etiological underpinnings of prostate cancer remain incompletely elucidated; however, a constellation of factors has been implicated in augmenting the risk of disease development:
- Chronological Age: The incidence of prostate cancer exhibits a positive correlation with age. While infrequent in men under the age of 40, the risk escalates markedly after the age of 50, with the majority of diagnoses occurring in men exceeding 65 years of age.
- Familial Predisposition: A positive family history of prostate cancer, particularly in first-degree relatives such as fathers or brothers, confers an elevated risk.
- Genetic Susceptibility: Inherited genetic mutations, notably in genes such as BRCA1 and BRCA2, have been identified as contributory factors in prostate cancer pathogenesis.
- Racial and Ethnic Disparities: Men of African-American descent exhibit a disproportionately higher incidence of prostate cancer and are more prone to developing aggressive phenotypes of the disease.
- Dietary and Lifestyle Influences: Dietary patterns characterized by high consumption of red meat, processed food products, and dairy, in conjunction with obesity, are posited to elevate prostate cancer risk.
- Geographical Distribution: A higher prevalence of prostate cancer is observed in regions including North America, Northwestern Europe, Australia, and the Caribbean, potentially attributable to variations in dietary and environmental exposures.
Clinical Manifestations of Prostate Cancer
In its nascent stages, prostate cancer is frequently asymptomatic. As the disease advances, however, a spectrum of clinical manifestations may emerge:
- Dysuria or diminished urinary stream.
- Urinary frequency, particularly nocturnal polyuria.
- Hematuria or hemospermia.
- Dysuria or a sensation of burning micturition.
- Erectile dysfunction.
- Skeletal pain affecting the hips, back, or pelvis, indicative of osseous metastasis.
- Unexplained weight loss or fatigue, typically in advanced disease stages.
It is imperative to recognize that these symptomatologies are not pathognomonic for prostate cancer and may also arise from benign prostatic conditions such as benign prostatic hyperplasia (BPH) or prostatitis. Consequently, a comprehensive medical evaluation is indispensable for accurate differential diagnosis.
Diagnostic Modalities for Prostate Cancer
Early detection is paramount to optimize therapeutic outcomes in prostate cancer. The following diagnostic procedures are routinely employed in the evaluation of suspected prostate cancer:
- Prostate-Specific Antigen (PSA) Assay: This serological test quantifies PSA, a glycoprotein produced by the prostate gland, in the bloodstream. Elevated PSA levels may be suggestive of prostate cancer but can also be indicative of other prostatic pathologies.
- Digital Rectal Examination (DRE): A manual examination of the prostate gland per rectum to assess for textural or nodular abnormalities.
- Biopsy Procedures: In cases of elevated PSA or suspicious DRE findings, a prostate biopsy is indicated to procure tissue specimens for histopathological analysis.
- Radiological Imaging: Magnetic resonance imaging (MRI), computed tomography (CT) scans, or bone scintigraphy may be utilized to evaluate for extra-prostatic disease extension or distant metastasis.
Staging and Grading Systems
Prostate cancer is subject to staging and grading protocols to delineate disease extent and aggressiveness, thereby informing therapeutic decision-making:
- Staging: Characterizes the tumor size and the presence or absence of metastatic dissemination. The Tumor-Node-Metastasis (TNM) system is the most widely adopted staging framework.
- Grading: Histopathological assessment of tumor aggressiveness. The Gleason scoring system is commonly employed, wherein higher scores correlate with increased tumor aggressiveness.
Therapeutic Interventions
The selection of treatment modality is contingent upon the stage and grade of the malignancy, patient age, overall health status, and individual preferences. Therapeutic options encompass:
- Active Surveillance: For indolent, localized prostate cancer, a strategy of vigilant monitoring may be favored over immediate intervention.
- Surgical Intervention: Radical prostatectomy, involving the extirpation of the prostate gland and adjacent tissues.
- Radiation Therapy: Delivery of high-energy radiation to eradicate malignant cells. Radiation may be administered externally via external beam radiotherapy or internally through brachytherapy (seed implantation).
- Hormonal Manipulation Therapy: Androgen deprivation therapy aimed at reducing circulating levels of male hormones (androgens) that promote prostate cancer cell proliferation.
- Chemotherapeutic Regimens: Systemic chemotherapy for advanced prostate cancer to target rapidly proliferating neoplastic cells.
- Immunotherapeutic Approaches: Immunotherapy to augment the host immune response against cancer cells.
- Targeted Pharmacotherapy: Utilization of drugs specifically designed to target defined genetic aberrations within cancer cells.
- Ablative Technologies: Minimally invasive modalities such as cryotherapy or high-intensity focused ultrasound (HIFU) to induce tumor cell destruction.
Preventive and Risk Mitigation Strategies
While absolute prevention of prostate cancer remains unattainable, certain lifestyle modifications may contribute to risk reduction:
- Adherence to a prudent dietary regimen rich in fruits, vegetables, and whole grains.
- Limitation of red meat, processed foods, and high-fat dairy intake.
- Regular engagement in physical exercise and maintenance of a healthy body weight.
- Abstinence from tobacco smoking and moderation of alcohol consumption.
- Informed discussion with healthcare providers regarding prostate cancer screening, particularly in the presence of established risk factors.
Prognosis and Survival Statistics
Prostate cancer generally exhibits favorable survival outcomes, particularly when diagnosed at an early, localized stage. Data from the American Cancer Society indicate:
- The 5-year survival rate for localized prostate cancer approaches 100%.
- For regional prostate cancer, where the malignancy has extended to adjacent tissues, the 5-year survival rate also approximates 100%.
- In cases of distant prostate cancer, characterized by metastasis to remote organs, the 5-year survival rate is approximately 32%.
It is important to note that for distant prostate cancer, 5-year survival rate for Black men is 29% and for White men is 33%.
Conclusion
Prostate cancer constitutes a significant health challenge for men; however, advancements in screening paradigms, diagnostic capabilities, and therapeutic interventions have substantially improved patient outcomes. Early detection facilitated by routine health evaluations and PSA testing is of paramount importance, especially for individuals with identified risk factors. Adoption of a health-conscious lifestyle and proactive engagement with healthcare resources are crucial for risk mitigation and the promotion of overall well-being. Individuals experiencing suggestive symptomatology or harboring concerns regarding prostate cancer are advised to seek timely consultation with a healthcare professional for personalized guidance and management.
Leave a comment
Your email address will not be published. Required fields are marked *